 Audits help us to deliver the best possible care by flagging up issues that might previously have been missed.
Audits help us to deliver the best possible care by flagging up issues that might previously have been missed.
If you’re new to audits, assisting with one for the first time could feel quite daunting, but as the Care Quality Commission recommends that all practices and providers take part in clinical and administrative audits, this is something that dental nurses would be well advised to get used to. The most common areas to be selected for audit are infection control, radiography and accessibility, but there are many other topics and specialities that could potentially be brought under scrutiny. If you’re completely new to the process, there are some great training courses available to take online, as well as plenty of information available for DCPs to look at beforehand. There are several CPD websites that offer courses on conducting audits and risk assessments, all designed specifically for DCPs and available to use at a very small cost. If you’re working within a larger organisation, there may also be training materials or courses available to staff, so it’s definitely worth asking your learning and development team about it. There is plenty of information on the NICE website regarding principles for best practice in clinical audit, and it would be useful to familiarise yourself with this before starting an audit.
When deciding how to perform your audit, you will need to consider the following:
Aim What is your aim? Usually audits are completed to see if treatments and services are of the recommended standard, and also to determine the overall quality of them.
Background Why are you completing the audit, and which techniques are you going to employ?
Who will be involved? The names of all nurses, clinicians and anybody else taking part will need to be recorded.
Standards Consider what you could do to improve your methods by comparing your own techniques to those listed under ‘best practice’. Use a tool such as SMART (Specific, Measurable, Achievable, Realistic, Time-based) to create goals for implementing any changes required.
Methodology What data you will collect? How many times you will collect it? What type of data needs to be collected and in what format (e.g. specially designed paperwork/programmes)? Data should be randomised wherever possible, although this does depend on the type of audit you’re completing. Data can be collected prospectively or retrospectively.
Analysis Compare results with standards set by previous audits.
Conclusion Identify any improvements or changes that are to be made, how these changes will be implemented, and any agreements or dates set.
Audit cycles
There are plenty of audit cycles and templates available online, and you could even create your own version that is more relevant to your practice and the type of audits you will be undertaking. However, the process always follows the same path of planning, audit and action. Here is a simple cycle that I have designed to assist with the process:

Audits that I have participated in
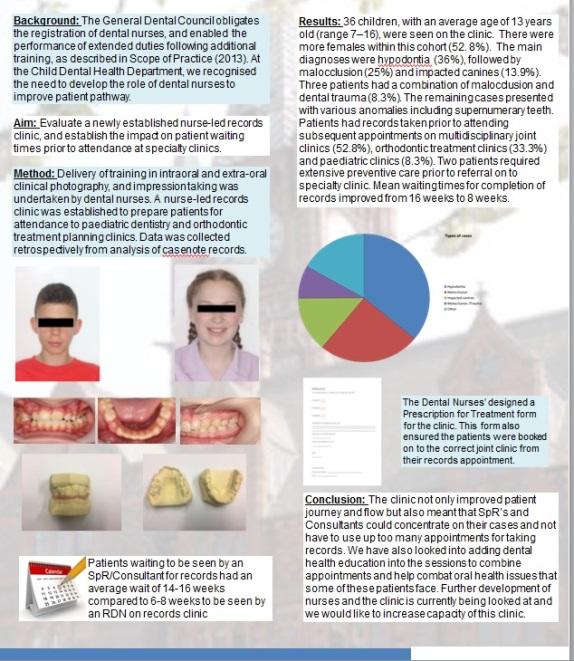
One of the biggest audits I have completed took place in 2017. Its aim was to find out how well a new clinic was running and determine whether we had been able to reduce waiting times for records appointments. The clinic was primarily set up to improve patient waiting times, so it made sense that we would audit it to see if we were achieving our goal. We also wanted to find out the reasons for patient referrals to the hospital and to see if certain conditions were more commonly referred to the records clinic than others.
I, along with another RDN, collected retrospective data from 38 clinics that had run over a period of 10 months. We specifically selected from within an age range of 6–16 years, as although we did have some patients attending this clinic who were older, we were completing the audit on behalf of the paediatric department. We recorded dates of attendance and patient numbers and then made a chart of this information before collecting the patients’ notes. After gathering the notes, we recorded the condition that each patient had been referred for and checked that they had attended their records appointment and had since been referred to the relevant joint clinic. All information taken from the notes was then recorded for analysis and conclusion.
We discovered that the clinic had been extremely successful and that we had been able to halve the waiting time for patients. We discovered that the clinic had improved patient flow and journey, and we were also able to see the types of cases we were receiving in the clinic and which was the most common. The findings were presented in poster format (see below) and submitted to the BSPD for their annual conference. We also have the poster displayed in our clinic so that both patients and members of staff can see the results.
I would like to repeat this audit in the near future, and this time include all orthodontic patients’ results as well. It would also be good to repeat the initial audit, as it has now been two years since the first one, and I think it would be useful to see if the clinic is still making improvements in waiting times and patient journey. It is always good to re-examine areas of treatment that have previously been audited to make sure that they’re still performing to the same standard and to see if any further improvements can be made.
If you decide to publish the results of an audit completed at your practice, remember to make sure that any patient data which makes them identifiable has been removed. You might have noticed that on our poster, we included headshots of our patients, but this was only possible after gaining patient/parent consent. It is also a good idea to make reference throughout your audit to the specific guidelines and principles, to remind yourself to keep adhering to them. Audits may seem daunting at first, but once you get started and become familiar with the process, they can be enjoyable and informative to complete, and can change the way you practice for the better.
Written by Beth Powe


